Your Fatty Liver Meal Plan
May 8, 2023 by Ginger Hultin MS RDN
Feeling overwhelmed after a new fatty liver diagnosis? You’re not alone. With so much (often conflicting) information out there, it can be hard to know what’s actually helpful—or where to even begin. The good news? Making meaningful changes to support your liver health is absolutely possible, and starting with a simple, realistic meal plan can make a big difference. Getting solid nutrition guidance early on is one of the most important steps you can take.
The liver is your body’s “metabolic hub”—it plays a key role in digestion, nutrient absorption, and storage. While heavy alcohol use is a well-known cause of liver damage, many cases of fatty liver disease are linked to diet and lifestyle habits. That’s why it’s so important to have routine medical testing done as part of your regular checkups. Catching signs of fatty liver early gives you the chance to make changes that can prevent the condition from progressing and causing long-term liver damage.
I always encourage my clients to ask their doctor to assess liver function annually—even if they feel fine. Early intervention is powerful, and working with a Registered Dietitian can be one of the most helpful tools for getting started. If you’ve been diagnosed with fatty liver, ask for a referral to a dietitian right away (sometimes you have to request it!). A meal plan tailored to support your liver can help take the guesswork out of what to eat.
Need support? You’re always welcome to reach out to me and my team—we’re here to help. Here’s a link to book a quick call to discuss.

What is fatty liver?
The liver plays a key role in lipid metabolism, movement, and storage. It makes digestive fluid (bile) for lipid digestion and specialized proteins (lipoproteins) for moving lipids throughout the body. The liver also processes dietary fats into energy and ships the extra away for storage in adipose (fat) tissue. Due to its role with lipids in the body, it is normal to have a small store of fat in the liver. In someone with healthy liver function, that’s around 5-10% of your liver is fat (by weight). Anything beyond this is “fatty liver” with severity dependent on what percentage of the liver is fat.
Sometimes, the liver is not able to process digested fat molecules correctly – this leads to a build-up of fat in the liver. Fatty liver can be classified as either nonalcoholic fatty liver disease (NAFLD) or nonalcoholic steatohepatitis (NASH) based on severity and the presence of inflammation and cell damage.
NAFLD is often called the “silent liver disease” as it tends to be asymptomatic and often will not result in permanent liver damage. The key distinguishing factor between NAFLD and NASH is the presence of inflammation and cell damage. NASH is defined as the presence of inflammation and damage in fatty liver. As the liver becomes increasingly inflated with fat, it becomes inflamed, cells begin to die, and the liver begins to lose function. This is what leads to unpleasant symptoms like liver/abdominal pain, severe tiredness, weakness, weight loss, yellowing of skin/eyes, spider-like blood veins, and long-lasting itching. NASH can lead to permanent scarring and damage, and in extreme cases, liver cancer and liver failure if you don’t get help and make guided changes. This is where dietitians are a great resource! Let’s look at the role of diet and other factors in how fatty liver can occur.
Your liver plays a key role in how your body processes and manages fat. It helps produce bile for digesting lipids, creates specialized proteins (called lipoproteins) to transport lipids hrough the body, and converts dietary fats into energy. It also stores a small amount of fat—which is completely normal. In a healthy liver, fat makes up about 5–10% of its weight. When fat content exceeds that range, it’s considered fatty liver, with severity depending on just how much fat has accumulated.
Fatty liver develops when the liver can’t properly process or break down fats, leading to a build-up within the liver tissue itself. There are two main types of fatty liver disease:
-
Nonalcoholic Fatty Liver Disease (NAFLD) – the most common type, often called the “silent liver disease” because it usually has no symptoms and doesn’t always lead to permanent damage.
-
Nonalcoholic Steatohepatitis (NASH) – a more serious form of fatty liver where inflammation and liver cell damage are present. Over time, this can impair liver function and may lead to more severe outcomes like fibrosis (scarring), cirrhosis, liver cancer, or liver failure.
With NASH, symptoms may eventually show up, including liver or abdominal pain, fatigue, unexplained weight loss, yellowing of the skin or eyes (jaundice), visible blood vessels, or persistent itching. While these symptoms often appear later, early detection and nutrition-focused care can help prevent progression and support healing.
This is exactly where a Registered Dietitian can make a big difference—helping you understand the role of diet and lifestyle in managing or even reversing fatty liver. Let’s take a closer look at how it all connects.
How does fatty liver happen?
There are several diet and lifestyle factors that can contribute to the development of fatty liver. It’s often linked with other health conditions that affect how your body processes fats and sugars, including:
-
High blood sugar or diabetes: When blood sugar levels are consistently high, the excess sugar gets converted into fat and stored in the body. Some of this fat can accumulate in the liver, especially if the liver’s ability to process and export fat is impaired.
-
High triglycerides or cholesterol: A diet high in added sugars and unhealthy fats, along with low physical activity, can lead to elevated blood lipids. When there’s more fat in the body than the liver can process efficiently, it can start to build up in liver cells.
One reason there has been an increase in fatty liver in the United States is that the standard American diet (SAD) is high in saturated fats, added sugars, and ultra processed foods – all of which have been shown to increase risk of health issues like diabetes, high cholesterol, heart disease, obesity, and overall disease risk. SAD is also low in vitamins, minerals, and complex carbohydrates (fiber). As many as 95% of Americans likely do not meet daily recommended fiber intake goals – this can be a major contributing factor to poor blood sugar control and excess fat in the body. With the prevalence of poor diet in the USA, it is not surprising that around 25% of Americans have NAFLD, and about 5% have NASH.
Unfortunately, it is also possible for there to be no clear reason for fatty liver to happen, and there are other components that are thought to contribute (like genetics or medications you have to take). This is another reason why regular health check ups and preventative/early lifestyle changes are so beneficial – you might have zero known risk factors and still have altered liver function which can progress and become problematic if not addressed.
The good news? Many of these factors are responsive to nutrition and lifestyle changes—which is why early intervention and support are so important. You can treat the factors that lead to NAFLD like high triglycerides, high cholesterol, high blood sugar/diabetes, and even reduce the amount of fat in your liver by consuming a well-balanced, anti-inflammatory plant-based diet – and I’m here to help you get started. This is the foundation of what myself and other Registered Dietitian Nutritionists do and how we help people. And I can tell you: it makes a huge difference.
Nutrition to support the liver
An anti-inflammatory diet focuses on eating a diet rich in nutritious foods that have anti-inflammatory nutrients like vitamins A, C, E, omega fatty acids, complex carbohydrates, and more. The foods known to be dense sources of these nutrients include whole grains, fruits and vegetables, and plant-based proteins.
Let’s take a look at how these nutrients support your health and liver:
Anti-inflammatory Micronutrients
Examples: Vitamins A, C, E, zinc, selenium, copper
Food sources: Fruits, vegetables, beans and legumes, nuts, seeds
Benefits:
- Act as antioxidants to help reduce liver inflammation
-
Support immune function and overall cellular health
Complex Carbohydrates & Fiber
Types: Soluble and insoluble fiber
Food sources: Whole grains, fiber-rich fruits and vegetables, beans and legumes, nuts, seeds
Benefits:
-
Help lower cholesterol levels
-
Promote fullness and steady blood sugar
-
Support a healthy gut microbiome
Healthy Fats
Types: Monounsaturated and polyunsaturated fats, including omega-3 and omega-6 fatty acids
Food sources: Nuts, seeds, avocados, olives, plant oils (like olive and flaxseed), beans and legumes
Benefits:
-
Help reduce LDL (“bad”) cholesterol
-
Support satiety and stable energy
-
Provide antioxidant and anti-inflammatory properties
Phytochemicals (Plant Compounds)
Types: Carotenoids, flavonoids, polyphenols
Food sources: Whole grains, fruits, vegetables, beans and legumes, nuts, seeds
Benefits:
-
Provide powerful antioxidant support
-
Help modulate inflammation and support immune health
Your Fatty Liver Meal Plan
Making a change to your habits and lifestyle takes time, energy, commitment, and thoughtful planning. Many people just don’t have enough of these to dedicate to properly investing in nutrition – and it can get overwhelming fast. As a Registered Dietitian, I am here to support you in these things to help you improve your nutrition with ease and confidence.
I am constantly developing quick and easy plant-based anti-inflammatory recipes for my clients to help reduce the amount of time spent in the kitchen while increasing their intake of important nutrients. I made this fatty liver meal plan to incorporate some of my favorite anti-inflammatory recipes to help take some of the pressure off of planning your meals, save time, and get great nutrition to support your liver health.
With easy access to the recipes included (linked below each week), you can efficiently make a list and head to your local grocery store and grab all your groceries for the week in one go. Then the fatty liver meal plan guides you through strategically using these great recipes, designed to leave you leftovers that you can take for lunch later in the week. No more constantly worrying what’s for dinner or raiding the vending machine for lunch (this helps you strategically use your leftovers as well).
This fatty liver meal plan was designed for you to be plant-based – a plant-based diet has repeatedly demonstrated its benefits for helping with blood sugar control, cholesterol management, and overall disease prevention. This is because plant-foods have high concentrations of anti-inflammatory, antioxidant nutrients and those nutrients that are “pro-disease” like saturated fats and large amounts of simple sugars are much less common in plant-foods versus animal products and ultra-processed foods. The foods I’ve included in your fatty liver meal plan were selected for their anti-inflammatory nutrients and abundance of healthy liver nutrients like B vitamins, omega fatty acids, antioxidants, and fiber.
Use this 3-week fatty liver meal plan to plan your grocery shopping, discover easy delicious anti-inflammatory recipes, and easily navigate your new approach to your diet, nutrition, and liver health.

Week 1 recipe links
Spicy Green Butternut Squash Enchiladas
Coconut Lemon Curd Overnight Oats
Pumpkin Spice Homemade Waffles
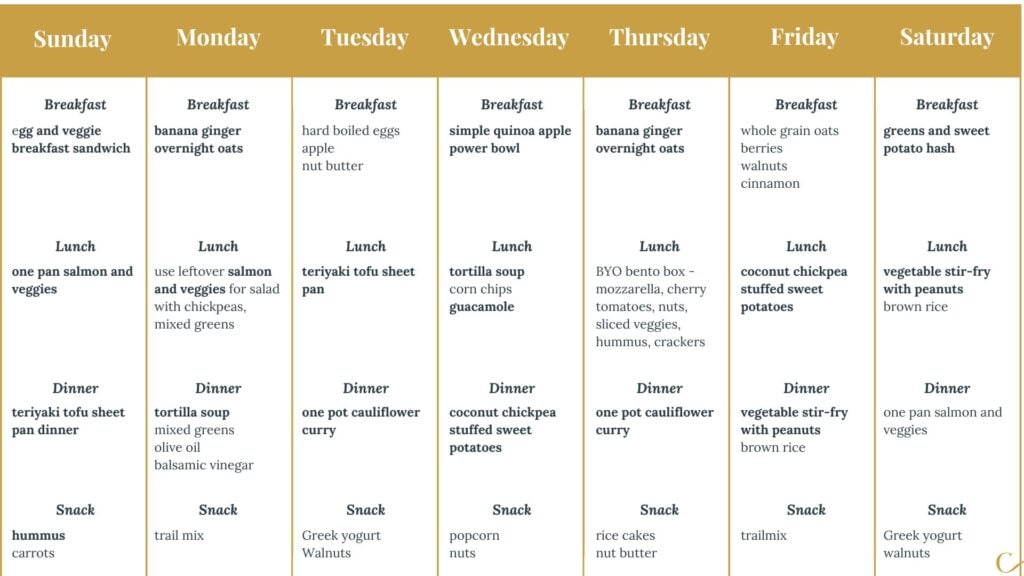
Week 2 recipe links
Egg and Veggie Breakfast Sandwich
One Pan Salmon and Veggies by Real Food Dietitians
Teriyaki Tofu Sheet Pan Dinner
Tortilla Soup by Feel Good Foodie
Simple Quinoa Apple Power Bowl
Coconut Chickpea Stuffed Sweet Potatoes
Vegetable Stir Fry with Peanuts
Greens and Sweet Potato Hash by Morton Salt
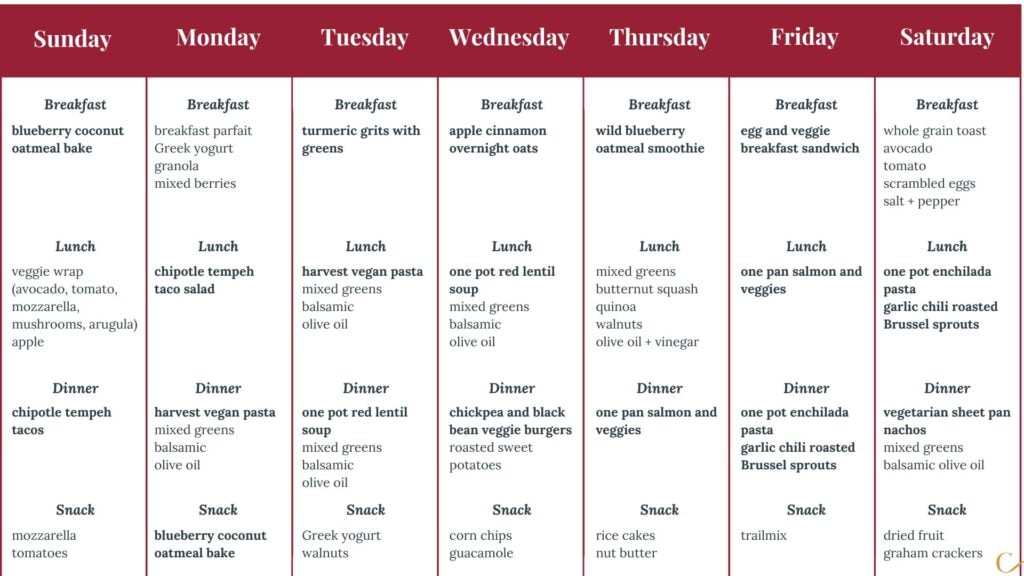
Week 3 recipe links
Blueberry Coconut Oatmeal Bake
Chipotle Tempeh Tacos by Oh My Veggies
Easy Vegan Pasta with Summer Vegetables (Harvest Vegan Pasta) by Dietitian Debbie
One Pot Red Lentil Soup by Minimalist Baker
Chickpea and Black Bean Veggie Burgers
Wild Blueberry Oatmeal Smoothie
Garlic Chili Roasted Brussels Sprouts
More NAFLD resources for you
For more resources on an anti-inflammatory plant-based diet, check out my ebook Anti-Inflammatory Plant-Based Eating 101. This is a great place to find more great recipes, information on benefits of plant-based approach, shopping and budget guides, and more meal plans for anti-inflammatory eating.
For in-depth, personalized support getting started on your anti-inflammatory nutrition journey, enroll in my Anti-Inflammatory Restart Nutrition Program: https://gingerhultinnutrition.com/resources/#program.
My Meal Prep for Weight Loss 101 ebook is another great place to start for helping build healthier habits with 4 weeks of pre-made meal plans and recipes, grocery list and tools for meal planning for yourself, and an overall balanced, healthful approach to healthier habits and weight loss.
Good luck, and happy cooking!
24 Comments
Leave a Comment

Ginger Hultin,MS, RD, CSO
Thanks for visiting! If you're struggling with a cancer diagnosis, autoimmune condition, gut health problems, or even a medical mystery, nutrition can make a HUGE difference in your day-to-day life. I run a virtual, concierge private practice where I partner with my clients over time to help them improve their health through nutrition. Be sure to visit the blog for easy, plant-based, anti-inflammatory recipes and our "Resources" page for a variety of self-paced programs, books, e-books, and nutrition podcast episodes.





Nice post
Thanks so much! I hope it’s helpful 🙂
I thought no salt is crucial for a liver diet?
Hi there! Well, you can’t do ‘no salt’ because there’s a certain amount of sodium needed to survive. You’re right though, a lower sodium diet is indicated for liver disease so I’d recommend sticking with a sodium restriction (always discuss with your doctor first, of course!) of 1500-2000mg per day.
Thank you. I discovered I have a fatty liver. Your discussion of fatty liver is informative. The meal plans are helpful. Interestingly, I’ve seen a longer list of associates conditions; I am overweight. I definitely need the support in turning things around. Thank you.
Oh I’m so glad this helps – I hope you can use the meal plans to start feeling better. Be sure to reach out if you ever need individualized support!
Ginger,
I like the meal plans. Is the variety necessary? Are the meals nutrient complete so that I can use 1 or 2 recipes from each of the meal plans (breakfast, lunch, dinner) and still help my liver?
I have the ingredients. Is the variety necessary?
Thank you,
JJ
Hi there JJ – great question! You know, you can use the outline of the meal plan to make it as simple or as varied as possible. If you want to just rotate in 1-2 and keep it very easy for yourself, that’s just fine. Consider mixing it up week by week so you get a variety of nutrients. Enjoy!
hi Ginger is there other food I can use that is not spicy? I have GERD and NAFLD?
Hi Hannah! Absolutely – I’d recommend using herbs like basil, rosemary, thyme, turmeric, cumin, dill, or oregano for flavor without spice. Hope that helps!
I have diverticulitis and fatty liver. I am constantly going back and forth with trying to figure out what I can eat and struggle with this daily. I’m having a flare up as we speak and have been in the hospital all evening in pain. What do you suggest eating for someone that struggles with both diseases?
Hi Joyce! Oh I’m so sorry to hear that; that’s very challenging and diverticulitis requires a special diet that changes as you have flares or not. This is absolutely a case for working 1:1 with a registered dietitian. Do you have one that you’re working with?
In my third pregnancy I ended up with a PUPS- like rash and was diagnosed with Cholestasis. The only thing that worked was going on a strict diet, even though I was eating very healthy already. I also did acupuncture to reduce inflammation. I’ve had several flareups since then. I’m wondering why someone would just start having so many liver issues if they’re not overweight, don’t drink alcohol, and eat a pescatarian diet. I just went back on a very strict liver detox diet, as this is the one thing that can help heal the liver; I’m just wondering if this is something that’s common.
Hi Jamie – oh that’s so frustrating, I’m sorry to hear it! It can be confusing when you don’t have the risk factors but you still have the condition. I hope you’ve got a great registered dietitian nutritionist on your team because I think it would help a lot 🙂
This is so wonderful thank you! I’m wondering if you have a printable pdf for the week plans? Thanks!
That’s a great suggestion, Sara – I’ll have my team start working on that 🙂
I abhor chickpeas . . . Can you recommend an alternative?
Hi Karen! Do you like any other types of beans? White beans or cannellini could be a good sub for you 🙂
I need help with this so badly
I hope this is helpful!
Hi Ginger
Thank you for your post.
I was diagnosed a year ago with fatty liver, and in April this year as celiac. Before that high blood pressure and insulin resistance with high uric acid. I guess is all part of the same… in Guatemala I haven’t found any support or a good practitioner, I feel like a rat lab, as if they were experimenting on me. It’s demoralizing
Hi Maru – I’m really sorry that’s happening to you – it’s a lot for anyone to handle. You’re right – there’s a lot of connections between all that’s going on with you, likely. If you ever want to pursue working with a professional like me for personalized care, you can book a discovery call on my site 🙂
Hey there, I was recently diagnosed with NAFLD, but I’m on the lower end of normal weight, borderline underweight. Due to stress and often forgetting to eat (associated ADHD), I’ve actually lost weight recently, unintentionally. That’s not a humble brag. I only bring that up because most of what I find is focused on losing weight and getting active. I definitely need to be more active, but I actually need to put on (muscle) weight, not drop it. Could you help with that? Can I still do that with this sort of plan here? Thanks in advance!
Hi Brandon – really glad you reached out and you’re right, my focus as a dietitian is not simply on losing weight but rather the changes to your diet and lifestyle that get you there. The plan here is designed for exactly what you’re working on and if you ever want to talk about a more personalized plan, you can book a call to discuss with me from my site 🙂